Introduction
[00:00:00] Detective Ev: All right. Hello my friends. I am back with my friend and fellow FDN practitioner, Becca Kyle. We are also both type 8s on the Enneagram, if anyone cares at all. I find a lot of people in our community of health actually do care about the personality type stuff and things like that. It explains why you guys like the other episode. It was a volcano mixing with another volcano, just bam, high energy.
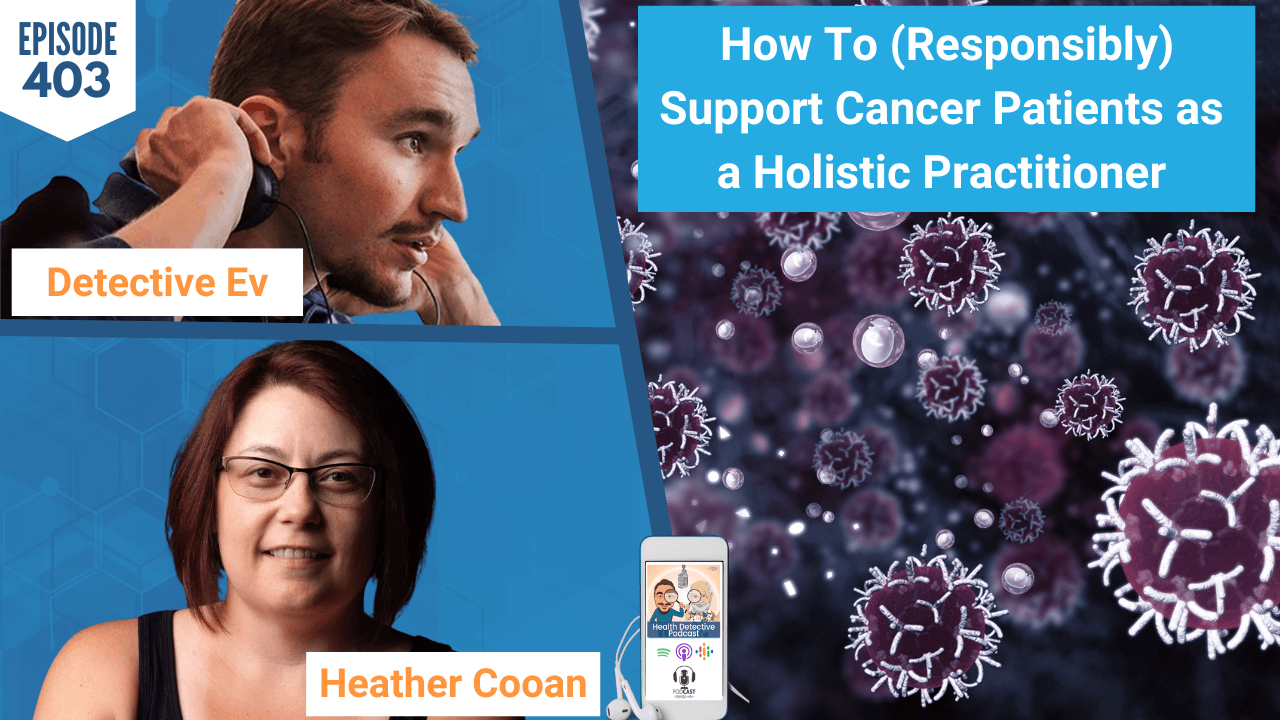
Today, I appreciate no judgment. I attempted to do my thing after coming out of the sauna. I thought I could pull off an episode after that and my hair said otherwise. I never really thought I’d say that on a podcast, but it needs to be addressed. The good news is we’re not here to talk about my hair. We are here to talk about my poop, though. It’s going to be even more interesting. What we’re going to be doing with my poop is analyzing Live lab results. You guys responded so positively to the episode we did with Ryan Monahan, where it was called How to Actually Analyze Thyroid Markers.
What’s funny is, and Becca obviously knows this as an FDN, we have access to utilize blood work with our clients. You could take our advanced course on that. But the truth of the matter is we don’t actually dive into blood work really, in any extent in the main course. It’s mostly under the premise that when most people come to us their labs kind of look normal or it’s not the biggest clue at the very least. The lab work is almost like, okay, cool.
Analyzing GI MAP Gut Test Results
We can give you a diagnosis with that if we were a doctor. But we’re not a doctor, so we need to look at other things to actually be able to help you at that core level. So, I’m figuring, they like that with the blood work that much for the thyroid markers, we really need to do this with the core labs we teach at FDN.
So today, we’re going to be talking about the GI MAP. It is something that, as I suggested already, is a stool test. We’ll talk about the technology behind it. I’m really here to talk to Becca cause she likes utilizing this test. It is one of the core labs we teach at FDN.
We’ll be going through all of these not in order necessarily. What I mean by that is it’s not going to be one episode after the other, but over the next couple of months touching on all of them, and it’s fun. So, if you are listening to this right now, you can catch us on YouTube. Just go to Functional Diagnostic Nutrition’s YouTube page and you can watch.
But we make these episodes with the audio listener in mind because our audience is way bigger on there. We will talk about this in such a way today that you do not need to see it, but some people are visual learners. With that said, I am going to share my screen and we’re going to bring this up for you here, Becca.
Of course, guys, I think I mentioned this, but if you want to hear Becca’s story, I’ll have that link in the show notes or the YouTube description. Today we’re here to hear her expertise about this test.
DNA PCR Gut Test Results
Becca Kyle: I love this test so much.
Detective Ev: And you can see everything just fine.
Becca Kyle: Yep. I can.
Detective Ev: Okay, awesome. All right, so this is from 2018. I’m doing a lot better now; don’t you guys worry. But the GI MAP was one of the things that when I went through FDN I actually did not end up running this. At the time they were not including this specific lab in the FDN course. Now, when you go through the course, included in your tuition, FDN will pay for it upfront for you even if you’re on a payment plan. You will have access to this test and a few others. It’s pretty cool.
Not that we have to like go crazy with it, but just to give people some context that might be completely unfamiliar with this, Becca, how does this lab work? Like what kind of technology is it using to analyze one’s stool?
[00:03:05] Becca Kyle: What I love about the GI MAP versus the original microscopy test that we were trained on is that I feel like it’s a lot more accurate. It’s not just a positive or a negative. It’s a DNA PCR test. So, instead of someone looking for organisms under a microscope, they’re looking for the DNA signature of the organism. They’ll be able to tell you is it below detectable limits, or is it high, or is it low, versus just present or not present.
But if something is super high to me, that’s going to warrant a little bit of a different action step or strategy than if something’s moderate or borderline, for example.
Gut Test Results to Widen the View on Health
I really love that it gives you the ability to just have a deeper understanding of how many organisms you’ve got going on in your body. It’s got some amazing digestive markers. In fact, I feel like most of the time that the digestive markers situationally may be my favorite markers on this lab.
It gives you a beautiful look at what’s going on in your microbiome. I think most of us feel in FDN, if you don’t have good quality gut health, you don’t have health. What other thing I love about this lab is it really talks to all the other labs. You know, it shows up on a DUTCH hormone test, what shows up on a food sensitivity test, which shows up on even an organic acid or HTMA test.
The data you get really is so synergistic with everything else, every other piece of data that you can come across.
[00:04:33] Detective Ev: Awesome. What’s worth mentioning is that very recently they changed the way this looks. Fundamentally, the test is almost identical. I know that they messed with some markers, but for the sake of today’s learning experience there is no reason that my test doesn’t work.
Of course, it’s just easier to use my own because I can absolutely share that without any problem. So, let’s go over the section. The first one, it just has these pathogens. Obviously, anyone watching this can see that it has every single thing in here below the detectable level.
But humor me. Let’s say something comes back for a client in the bacterial parasitic, or viral pathogen section. Big picture approach, how are you looking at these things and addressing them?
Gut Test Results: Pathogens
[00:05:10] Becca Kyle: Well, I feel like the ones that show up on the first page are what I would call like pretty hard core. If something shows up on this page, we want to really pay attention to it and address it in significant ways. Because something like Giardia, for example, can really cascade into so many health issues. It can even impede your body’s ability to absorb B12, for example.
There are so many things on this first page that we would not want to just be like, eh, it’s fine. No. We address it, and we address it quickly. Because it can, like we said, be implicated in so many of your chronic symptoms, but also really just the underlying large amounts of inflammation and toxic burden even.
[00:05:53] Detective Ev: Sure. So, I happen to pass the test on this one. We are good on this page.
I will be honest, a lot of the clients that I’ve worked with throughout the years have actually historically come up pretty clean on this section. That’s not always the case. We train you what to do if you go through the course if someone comes up on this stuff. But when I’ve even seen it, the good news is a lot of the things were actually correlated with what would’ve been like food poisoning. It was a transient thing, and it passes through them.
But yes, like Becca mentioned, I mean the giardia, certain of the parasites, especially not so great. And depending on what shows up in the bacterial pathogen section, could be not so friendly.
I’ll jump right down to the next section.
Gut Test Results: H. Pylori
Again, for those on audio, what we’re looking at now is a section known as H. Pylori. We see H. Pylori itself as the result, and then there’s a bunch of virulence factors.
Let’s say Becca, maybe I’m a client of yours, right? I haven’t heard of H. Pylori at all, and I get these results back. How would you break this down for those people?
[00:06:44] Becca Kyle: Yeah. H Pylori is really common. I would say probably 80% of my clients end up having it. It’s a bacterium. It can have a positive role in like ulcers and gastritis and some more severe kind of diagnosis. However, in my opinion, we’re looking on a deeper level.
We’re looking at the fact that it can lower your stomach acid, which should be your first line of defense against anything else ingested, like you come across a bacteria or pathogen. Basically, it’s like if you have H. Pylori it can have the potential to kind of be in your stomach and your gut area.

Like you leave for vacation, and you leave all the doors and windows open in your house and say, hey, come on. Let’s go invade. I always say it’s like the mob boss of the gut. If you don’t have it, then it’s always, to me, good news. If you do have it even on, like you see here on yours, that yours is not what we would consider high.
The thing about H. Pylori though, it often hangs out in the more upper regions of the gut, in the stomach area. By the time it gets down into a stool sample, it might actually be higher in the upper regions of the GI tract.
H. Pylori Spreads Via Saliva
I always look at H. Pylori as a huge healing opportunity because of its ability to lower stomach acid, to allow other bacteria and pathogens into the gut, and then it can potentially, with that lowered stomach acid, reduce your body’s ability to even absorb protein. There’s some correlation with low elastase, which we’ll look at on that last page. And it can just be implicated in a lot of chronic issues.
To me, I have a lot of clients that shows up, probably almost always shows up when someone has anxiety, insomnia, things like the neurological issues because it can impact your body’s ability to make these amino acid-based neurotransmitters, the feel-good hormones. They make you feel happy and balanced and all that stuff.
H. Pylori can, if you’re going back root cause and kind of backtracking, it can have a causative role in an imbalanced mood even. So, I look at H. Pylori as a massive healing opportunity. Even though it’s not high on this lab, I would still address it.
It’s very common that it’s spread in families or with a romantic partner because it’s spread very commonly via saliva. It also hangs out in your oral cavity. If you’ve got someone that you’re loving on or you’re sharing a toothbrush, or you’re sharing a straw or spoon, I always recommend that the whole family or whoever is involved there also address it for themselves.
[00:09:09] Detective Ev: It’s a tough thing because H. Pylori, once it is there, it’s a little tricky. Many people thankfully, are asymptomatic. It’s estimated that about 50% of people in Africa actually have H. Pylori.
H. Pylori Could Be Much More Prevalent
This is what’s really fascinating to me. The estimations are always around 20% to 30%, at least by Western medicine, that that’s how many people have this in the United States of America. I’m not even saying that that’s so far off. Let’s say it’s almost completely wrong, and it’s 50% of Americans. What you mentioned before was brilliant about the idea that 80% of your clients show up with H. Pylori.
I have found the same thing over the last five and a half years. I would even estimate, I mean, literally the actual number for me is probably 90%. Then of course we are talking about stool testing, which is an imperfect measurement. There are chances that if you and I run enough of these, we are going to miss something like H. Pylori and it’s going to come back up as a false negative, which is fascinating.
So, there’s only two things that can be happening here. Either this is way more prevalent than we think, which I think is possible, but that still does not account for the numbers that we see. Ten the other side is that this is, even though correlation isn’t causation, it’s something that seems to be par for the course when someone is ill.
You can simply argue that when people are super stressed out, which most people are, if they’re chronically ill, this gives a great ground for something like H. Pylori to hop on in. I mean, if a fraction of the population has it, eventually you are going to be exposed to it in that stressful state and it can come and make its home. I mean, you could spend all day trying to theorize why this comes in, but it’s not something to mess with.
Reduce H. Pylori to Get Rid of Symptoms
I don’t know if we ever got to talk about the virulence factors that can be associated with a higher risk factor for like gastric cancer and stuff like that. I was symptomatic to be clear. Becca wouldn’t have known these things, so I should have mentioned this.
We always correlate with the symptoms that the person is dealing with. Thankfully by 2018 I was doing a lot better. But I was coming off of having pretty severe cystic acne. I definitely had sleep issues when I was younger. A panic disorder, major depressive disorder, GERD. I was diagnosed with that at 15.
[00:11:16] Becca Kyle: I can’t tell how many of my clients have reflux and are on reflux meds. They come to me and they’re like, Becca, I don’t want to be on these meds. I would say 98% of the time, H. Pylori shows up. Get rid of the H. Pylori or greatly reduce it, and they can get off their meds. It’s their own desire to do so.
Cause I, as an FDN, we don’t tell anyone or suggest to anyone that they get off meds. But if it’s there something that they want to do, almost every single time they can’t because H. Pylori also has a causative role in things like reflux or GERD or heartburn, things like that.
When you went through your protocol, how quickly did your symptoms improve?
[00:11:55] Detective Ev: Well, it’s interesting that you said that because one of the things that I did was I utilized Matula tea. I always laugh about Matula tea because it comes from South Africa, but the website that they use is very outdated and the tea is extraordinarily expensive comparing to most teas.
Gut Test Results: H. Pylori’s Virulence Factors
It’s almost funny for people because they’re like, really, this is what you’re sending me to do? This is what I need to go buy? But it’s one of the more effective things and has a high level of efficacy in our world at least.
I used that, and I would say within a month and a half, now I’m including the month that I did the Matula tea, I started to notice the skin get better and things just start to feel better.
What’s really interesting, it’s a point I want to go to with something you mentioned. You talked about, you noticed how people might be able, voluntarily, of course, to get off these medications if H. Pylori is gone or greatly reduced. I have noticed a ton of validity to the latter. In your experience, you have found that if people can get this lower than maybe what they came to with originally, they can still see that symptom relief. Is that correct?
[00:12:55] Becca Kyle: Yes, most definitely. Sometimes, depending on the level that you have, it might take more than one round of some herbal protocol to be able to maybe have it show up below detectable levels on a retest. But the goal is to bring your levels down.
Then of course we look at the next section, it’s about balance. If you’ve got H. Pylori and super low levels of your normal good guys, you’re going to be super imbalanced. We bring down the level of H. Pylori, bring up the levels of your low good guys, and you’re going to have, typically, fewer symptoms.
Yeah, with this virulence factor, it basically has the potential to increase disease in the body. It’s like doubling it up or tripling it up.
Gut Test Results: H. Pylori, Stress, and Symptoms
Now your specific one here, this virB one, unless you also have the cagA, it’s typically less likely to change the clinical outcome of an H. Pylori infection. But yeah, the virulence factors can make your symptom presentation much worse and has the potential to increase the disease potential of the bacteria.
[00:13:59] Detective Ev: I did not even know that myself, so thank you. That makes me feel good.
I will say too, everyone needs to figure out what’s right for them. And if you go through the FDN course, if the client wants to, we would aim that it’d be eliminated, that would be great. I have found that if I am addressing the other things in my life correctly, this does not seem to matter. But it is my belief even without a current retest that I probably still have H. Pylori.
There are two reasons I believe that. One, in the last four years, I don’t know why I would’ve said it on this podcast. I’m not someone that personally believes in going out and just hooking up with random people. And with hair like this, you know, I can only swing them every few years anyway. No, I’m kidding.
But I’ve dated two women since 2018, and I would assume that based on what we’ve seen, H. Pylori was probably present in at least one of these women. So, I know I’m getting exposed again.
What I saw, Becca, which is really interesting, is like, this was just last year. I feel really great nowadays, which is great. But last year when I was pushing the schedule a little bit and I was accepting more speaking stuff than I should have, I started to get symptoms when I would eat ginger or certain other foods.
H. Pylori Asymptomatic from Just Addressing Lifestyle Issues
I never got a diagnosis. This is someone, I made a choice on my own because I felt that I knew what was happening. It appeared to me that I probably had a low-level ulcer because there were certain things, very specific ones, that were triggering pain. The pain would happen at certain times. It was relieved in certain ways, and I was like, whoa, man, I’m pushing a little too hard.
Now, I never went through some Matula tea protocol. I didn’t do all this crazy stuff, but I did do the lifestyle things that I know I should have been doing anyway. I stopped pushing like a maniac and I went through some basic protocols. So, if I tested right now, I would almost bet money that H. Pylori is president in my body, and yet I’m asymptomatic again. I feel good.
I’m not pushing an idea that we shouldn’t try to get rid of it. I mean, that’s great. It doesn’t seem to be particularly helpful. But it’s also one of those things that it is such a nuisance and so prevalent, you can learn to work with it more or less by addressing the lifestyle stuff and doing other things.
But you might be symptomatic again. And I do believe I’ve been symptomatic because of it. Again, honestly, I don’t think it ever fully left my body.
We go down to the next section, talking about Normal Bacterial Flora. We see a lot of lows here for mine. Especially now knowing what I was dealing with, coming off of some cystic acne, severe mental health issues, things like that, what would be your interpretation when you see things this low after all these years?
Gut Test Results: Normal Bacterial Flora
[00:16:24] Becca Kyle: I would say that you have a really decent size imbalance in your gut flora. I mean to keep it simple with my clients, I tend to say good guys and bad guys. It’s pretty basic speech I suppose.
These are bacterial flora that you want in your gut. They’re so important. They make serotonin – feel good hormone. They make melatonin. They make vitamins. They help keep your estrogen balanced. They are what you want.
Another kind of basic thing I say is that in the gut we have this communication highway between our gut and our brain. It’s called the enteric nervous system. We want the good guys to have the loudest voice, versus the bad guys, you know? So, when you have this imbalance of some present H. Pylori, and we’ll see what else you got going on here in a little bit, and low good guys, who’s going to have the loudest voice? It’s these opportunistic pathogens that cause a lot of your symptoms.
So, I would say based on this lab that you definitely needed to rebalance your normal flora. This is such a, again, a significant healing opportunity in the body because these gut bacteria are so important for so many things. If you simply don’t have the amount you need to do all these beneficial processes in the body, that can look like a lot of chronic symptoms.
What you showed up here with all these low bacteria, would you say that correlates with how you were feeling at the time?
Low Good Guys Make Your Gut Vulnerable
[00:17:49] Detective Ev: Of course, cause you know, it’s one of those things where even if I got a lot of the major symptoms out of the way, it’s amazing how sick we can actually be, is what I’m trying to get at.
I thought, and in a sense, I was doing much better than I had been previously in 2018. But like now, it’s like, okay, I’m back to how I really wanted to feel like. You know, I can go work out five, six days a week. I’m doing boxing, I’m strength training, I’m still speaking, I’m doing all this stuff. I’m not saying everyone should push themselves all the time, but I felt like I was missing some of that resilience that I had.
So yes, not only does it correlate with that, but one thing that I omitted today, Becca, was the fact that even though I hadn’t been on antibiotics in several years at that point up until 2018, before the age of 18, I had been on over 20 courses of antibiotics, some of which lasted a month or longer.
[00:18:33] Becca Kyle: Wow. Okay.

Well, that definitely correlates with what shows up on this lab here. So many of us, if we had to do that growing up or whatever, didn’t necessarily take the steps to repopulate your good guys, after a round of antibiotics, you’re just cycling kind of this downward spiral of imbalance of low good guys. When your good guys are low, it’s also kind of like opening up the doors and windows of your house and saying, come rob me.
Time to Feed and Reseed
Your good guys are really a service and protective measure in the gut too.
I would say definitely I see a need here for some repopulation so that we can feed and reseed. You know, reseed with good bacteria, that would be probiotics. Feed them with their food, which would be the prebiotics.
I love all the great, amazing, simple, cheap prebiotic foods you can get out there. I’m not one that typically encourages people to buy bottled supplement prebiotics. No, just eat the prebiotic food. What do you typically do? Sometimes it’s easier just to pop up a prebiotic supplement, but do you prefer to get your prebiotics through food?
[00:19:34] Detective Ev: Well, first of all, I love that you recommend that for clients. I think that makes this work a lot more attainable for people, right? It’s much cheaper. I mean, everyone has to eat. You’re going to have to eat some foods anyway, so to incorporate those make sense.
And yeah, obviously my diet had changed pretty dramatically at that time. I am an advocate for sure, personally, if my clients can afford it, I love sending people almost routinely through the Total Gut Restore by Microbiome Labs. I’ve seen so much success with that, and I actually have gone through it multiple times. I always use MegaSpore, but I’ll keep throwing it in. I mean, yeah, if we could start naturally, that’s great.
I think for me, listen, it was not natural at all to take 20 courses of antibiotics. So, this is the other side of this.
Good Guys are So Low, Need Some Extra Support
I was doing a lot of the things that I thought were right almost for four years prior to this test, and I still wasn’t where I needed to be. I’m sure with certain people, especially if antibiotics hadn’t been in the mix as much, you kind of destroyed it naturally in a sense. So, maybe you have a better chance of fixing it up.
We really don’t know what 20 courses of antibiotics does to someone. There’s not really science showing what that’ll do long term. So, since I got affected unnaturally, I almost try to help myself, I’m using the word loosely, but in an unnatural way cause obviously there’s nothing natural necessarily about taking a bottled supplement like you mentioned.
[00:20:46] Becca Kyle: Well, and there’s a time and a place, by all means.
Especially, let’s say maybe you had some low normal, but your phyla microbiota was fine. Then maybe I might be like, let’s do this with food. But your phyla microbiota both of them were low. And these are good bacteria that dominate your entire digestive tract, from your mouth to your colon.

So, when we see low across the board like this, and even like one is not even there, then yeah, I would say that for someone like you, you need a little bit of an edge, a little extra support. You may be using some of these prebiotic foods, you know, jicama, green banana flour, Jerusalem artichoke, could be more of a potentially long-term maintenance situation.
Let’s get these good bacteria flourishing and then you can maintain with some prebiotic foods and whatnot.
Commercial Break – 12 Days of Christmas Special
[00:00:00] Detective Ev: Hey guys, it is Detective Ev here with some good news. The team that does the podcast asked me to record some exclusive content. What we did is a 12 Days of Christmas Special where we record 20-minute episodes with some of our top FDNs, as well as Reed Davis, the founder of FDN.
We only dive into the deep stuff. No formalities, no bios, just tips to actually help your health and or your business. We have about six episodes on the business side, and then six advanced health tips ranging from secret gluten sensitivities and how to deal with them around the holidays, how to deal with mold exposure. We got all this good stuff.
What you want to do is go to fdntraining.com/insider, that is fdntraining.com/insider. There you can sign up for that podcast. It is not going to be released to the public. It is only for people who are registered. You will have it dripped into your email for the 12 Days of Christmas. That is fdntraining.com/insider, and you can check out the link in our show notes as well.
All right, now back to today’s episode.
Gut Test Results: Opportunistic Bacteria
[00:21:33] Detective Ev: Awesome. Now moving down to this section here. We’re looking at, for those on audio, opportunistic bacteria. Then the subsections under that are Additional Dysbiotic/Overgrowth Bacteria and Potential Autoimmune Triggers.
This one is not as lit up as some of the other sections. So, what’s your interpretation on this one?
[00:21:51] Becca Kyle: We definitely see some bacteria that are there that aren’t going to do you any favors. I would consider the bacteria that shows up in this section to be pathogenic. They only cause disease. They’re not going to help you in any way, definitely not.
I’ve seen this show up with like, 10, 12 in the high range. You have one in the high and then three that are present otherwise. But I would say that again, it’s about balance. You don’t have a ton on this opportunistic bacteria section, but you did have low good guys.
Again, when we look at the scale here of good guys versus bad, I always kind of think of like an old Western movie, right? Like good guys versus bad guys. Again, we want it to be balanced. Even though you don’t have a ton show up, because your good guys are so low, again, who’s got the loudest voice here? Who can do the most damage?
I tend to see a lot of this can be caused by constipation. That can be caused by you get these in your gut because of that low stomach acid. And that prevotella too is really correlated with rheumatoid arthritis. Were you experiencing joint pain at the time of this lab?
[00:22:59] Detective Ev: Thankfully, that’s one of the things that I’ve never really had.
Be The Brains Behind the Tools
[00:23:03] Becca Kyle: Okay, good. I have some clients who come to me and they’re like, I don’t have any gut symptoms. My gut’s fine. I have a lot of neurological symptoms, you know, but this will light up like crazy.
What we have to do as FDNs is correlate it back to the person. So, I would address these in a GI MAP protocol, a little bit of Biocidin. You know, it’s nothing like, oh my gosh, this is so crazy. But some of these bacteria can still create symptoms, whether it’s bloating or IBS or constipation. They still have the potential to cascade into symptoms that you’re experiencing.
[00:23:35] Detective Ev: Sure. There are two really interesting things that you’re doing here that I hope people that listen to this, that might not be FDNs are starting to pick up on. One is the fact that if you are actually looking at this test right now, there’s only one thing here labeled high, but there’s many things that we don’t necessarily want.
The labs are tools. They are fantastic things. They’re great to use. But we need to be the brains behind those tools. Just because a lab might consider like even H. Pylori, right? It didn’t have H. Pylori as high because it’s a lab. It’s basing it off something else. We, in a perfect world, don’t want that in someone at all. So, you could argue that any amount of H. Pylori is quote/unquote “high”.
Then the other thing that you’re doing is the clinical correlation. If people really understand this, they understand the fundamental difference between a Western medicine practitioner and an FDN practitioner. There are a few differences, don’t get me wrong, but this is the fundamental one.
Difference Between a Western Medicine Practitioner & an FDNP
When a Western medicine practitioner gets test results back, they are looking to diagnose something. That is what they’re trying to do. If your blood sugar was XYZ level over a couple times, you could get diagnosed with Type II diabetes.
We cannot diagnose or treat anything just as FDNs. If you’re a doctor and an FDN, of course you could do that. But as FDNs, we cannot do that. What we are doing is clinically correlating and you guys will notice how Becca did exactly what she’s supposed to do. She asked me, well wait, did you have this joint pain at the time in this case? No, I didn’t have that. Okay. That doesn’t clinically correlate for Ev.
Other people, and in fact most of the time, you will find that you can pretty much guess a lot of the times what their symptomology might look like based on what shows up on the labs. But it’s not always there because everyone is an individual and everyone has their own unique thing going on. Just something to note for people that are listening today.
We have the Fungi and Yeast section. Thankfully at this point in time, I didn’t have Candida show up. Of course, it could be a false negative. But I fell into, before the world of FDN, a lot of those cleanses and stuff, like the Candida cleanses. Even if that wasn’t a complete protocol for the whole body, I feel like it might have helped with there.
But I’m sure you see Candida pop up pretty frequently on tests, I’m guessing, right?
Gut Test Results: Fungi/Yeast & Parasites
[00:25:37] Becca Kyle: I do. It’s just so common too. Cause we think of Candida as a secondary organism. It’s the little brother, a little sister. When you have something like H. Pylori or opportunistic bacteria or parasite or something like that, Candida likes to hang out. You know, it’s always running after saying, hey, I want to play too.
We rarely see Candida on its own with nothing else on the lab. But it is very common to see it hanging out with the other guys.
[00:26:01] Detective Ev: Right. I will skip over that section. We don’t need that right now cause I wanted you to talk about this. On the Parasite section we see something called Blastocystis hominis, and it is high. This is something we are well trained on as FDNs.
What is going on with this Blasto thing for me?
[00:26:17] Becca Kyle: I just like to call it Blasto because it just makes me feel good to say Blasto. I shake my fist at it.
Blastocystis hominis, it’s a parasite, it’s a protozoa. Typically spreads through fecal contamination of food or water. When I say that to someone, sometimes they’re like, but I’m not doing anything gross. It doesn’t mean you’re doing anything gross. Maybe you ate at a restaurant, they didn’t wash the produce properly, or you just don’t ever know what you’re going to come in contact with.
Which is why, as Evan stated before, always addressing that lifestyle and keeping your stress levels down and keeping your body able to deal with this stuff that as we come into contact with it.
Gut Test Results: Blastocystis Hominis
Clinical implications of Blasto can present Ev with diarrhea, abdominal pain, nausea, vomiting, irritable bowel syndrome, all sorts of things. So, with your symptom presentation at the time of this test, were you experiencing any of those symptoms of it?
[00:27:10] Detective Ev: Interestingly, I never had the constipation thing. I would occasionally have some diarrhea.
One of the things that I got historically, and thankfully it was lessened over time and not even present anymore, but one of the things that made me run this test actually finally, even though I’d been an FDN for a little bit, was the idea that I got this severe stomach pain that ended up landing me in the hospital.
They looked at this as completely benign. But I mean, I was going in there 20, 21 years old and was basically told I needed a back-to-back endoscopy and colonoscopy. This sucked. I was in the hospital for three days, endoscopy, one day, colonoscopy the next, or maybe it’s reverse order. I don’t know. Either way, I got tubes in places I never wanted tubes, and I had it back-to-back.
I would assume that that is probably part of that picture because again, they couldn’t figure out anything. They just sent me home eventually, and I had to have all these expensive things done on me because of the severe stomach pain I was dealing with.
[00:28:03] Becca Kyle: Yeah, it’s a pretty nasty booger. When I see this show up on a lab, I actually get really excited cause I’m like, this is a massive healing opportunity potentially. Part of the issue with Blasto is that it can be difficult to eradicate. Of course, none of the things we do are quick fixes.
Bringing Down Inflammation & Balancing the Immune System
None of what we do is meant to be a quick fix. But definitely some herbal protocols just like we have bacterial protocols for H. Pylori or the pathogenic bacteria, we also have parasitic protocols as well that allow your body to deal with these. Supporting the immune system, you know, supporting detoxification, all the things we would do in order to allow your body to take care of these bugs.
I always think of those, I mean, I’m a lot older than you, but those old Raid commercials, like Kill Bugs Dead. Maybe you don’t even know what I’m talking about.
[00:28:54] Detective Ev: Yes, I vaguely have an image of it.
[00:28:56] Becca Kyle: It’s alright. But I would look at this high level of Blastocystis hominis as a massive healing opportunity for you. Even if you maybe potentially, let’s say you weren’t having some of those clinical symptoms, it can still significantly drive inflammatory processes in your body.
One of the things we do with FDN is we are trying to bring down inflammation or trying to balance out the immune system and allow your body to function at an optimal level. So, taking care of this Blasto, whether you’re symptomatic or not, would be very important.
Then Blasto also has some clinical implications as one of the potential triggers for Hashimoto’s. When I see someone with thyroid issues and Blasto, we definitely want to support them and support their bodies in eradicating this little parasite.
[00:29:43] Detective Ev: Interesting. Yeah, Ryan Monahan, that was huge in his story. When he got rid of Blasto, it’s like his thyroid symptoms changed pretty much overnight, which is awesome.
Getting Rid of Blasto Can Be a Long-Term Project
With this said, one of the only other markers that we’ve really hyper focused on was H. Pylori. We had given the audience a conclusion, just an opinion, not necessarily a rule. But if you did get this lowered and it stuck around, it might not be the worst thing in the world, and you could just kind of carry on throughout your life.
When you see something like this though, you’re going to want this gone on a retest ideally, right? You don’t want this necessarily hanging out?
[00:30:12] Becca Kyle: No. And with something like Blasto, typically I would encourage someone to do about a 90-day parasite protocol. It may take longer than 90 days. When someone shows up with Blasto, I let them know what the expectation is, it’s a long-term project.
You know, it’s facilitated. It’s bringing up your good guys. It’s eradicating. So again, supporting the detox process to allow your body to support your immune system, to allow your body to be able to handle this, and allow those herbs to work. But it definitely can take longer than 90 days.
If you had a different parasite show up, that might be a little bit easier to kind of get rid of in that 90-day process. But then again, that’s why we retest for certain for these. So, we can see what’s going on and what your levels might be after a protocol. Maybe your body is just super awesome, and it dealt with it in 90 days, but maybe not.
So, definitely don’t want this hanging out though. Absolutely not.
Worms May be Less Likely to Get Caught
[00:31:04] Detective Ev: Cool. All right, thank you. Next section here is going to be, well, subsection. Honestly, I have never run one test yet where I have seen Worms pop up on the GI MAP.
Becca Kyle: Me neither.
Detective Ev: Is this something you see?
Becca Kyle: No. Never.
Detective Ev: Got it. All right.
I think for the sake of today, at least just for time, we can kind of skip by it, but we could mention something about it if you’d like.
[00:31:23] Becca Kyle: Well, I think with worms too, they tend to be bigger than say, like a bacteria. So, you can have a lot more colonization of bacteria in that stool sample where a worm might kind of not be in the part that you scooped up and put in the samples. I think it’s just, they’re less likely to be caught per se in that stool sample. But that’s just my own opinion on the squirmy worms.
But also too, if we’re addressing like a parasite or something like that, oftentimes if you did have a worm, it has the potential to take care of that as well.
[00:31:51] Detective Ev: Thank you. Then the last real section here is Intestinal Health. The subsections for those on audio is Digestion, GI markers, Immune response, and Inflammation.
There are a few obvious issues here on mine. We’ll just break them down one by one.
[00:32:08] Becca Kyle: I love these. This is, again, I think I said earlier, one of my favorite sections of the test.
Gut Test Results: Elastase-1 and Steatocrit
So, digestive markers. We’ve got something called Elastase 1 which is a pancreatic enzyme that facilitates the digestion of protein. At 649, I would say you’re doing good. We don’t want to really see it under 500.
If it’s below 200, then you potentially really could have some issues digesting, absorbing your protein, which is important for blood sugar and hormones and muscle growth, all the things. But your Elastase 1 looks great.
It’s also very common with maybe more on the higher side of H. Pylori to have low Elastase 1. Those two tend to correlate a little bit. Your Steatocrit was below detectable levels. Steatocrit is a marker for undigested fat in your stool. So, Evan, you were doing fine with this marker.
If you had some positive numbers on this marker, that can be implicated in a lot of things. You need dietary fat for satiety to keep you fuller. Obviously, you want to be absorbing that. You need it for hormones, dietary fat, and that cholesterol is the precursor for all your hormones. Your brain needs fat.
But on your lab, you seem to be doing a good job of digesting and absorbing your fat. It’s not going through to your stool sample. So overall, I would say your digestive markers look pretty good here.
[00:33:19] Detective Ev: Awesome.
It is worth mentioning for those listening. I personally have used digestive enzymes long term. You know, it’s something as an FDN you can kind of decide what you want to do because it reads clear as day about it in the course that there is a potential downside to using digestive enzymes long term in that they might make your own natural ones not as effective as they could be.
Gut Test Results: Beta Glucuronidase
But to me, with our high stress lifestyle, with everything I’ve been through with the antibiotics, it was a personal choice. I still use them to this day. I don’t know if that influenced these results at all. But either way the GI MAP’s interesting because it’s like, okay, well sure it’s a snapshot in time. But it’s also saying like, even if you’re using supplements, what are those supplements leading to? If it’s leading to overall good results, then that’s probably an okay thing and something I’m willing to stand by because I feel like I’m doing pretty good.
The next little section here says GI Markers, but really what they’re looking at is something called beta Glucuronidase. It’ll look like b Glucuronidase on video and then Occult Blood. My Occult Blood is super good. But the beta Glucuronidase is starting to get a little high there, isn’t it?
[00:34:16] Becca Kyle: Yeah. This is actually one of my favorite markers on the entire test because I see it clinically correlate so well.
Beta Glucuronidase is actually naturally produced by your liver, your kidneys, and intestinal epithelium. But it can also be produced in excessive amounts by pathogenic bacteria in your gut.
What happens when your beta Glucuronidase is high, is that it can disrupt your body’s ability to detoxify toxins and especially hormones. So, think of your liver as a full bucket of toxins and hormones and stuff that’s trying to dump out. It tries to dump them out, but if your beta Glucuronidase is high, it’s like someone taking half those toxins and hormones and dumping them right back in. So, you tend to be recycling estrogen and recycling hormones.
The Body’s Need to Detoxify is Huge
When I see this number high, it’s a good bet that you have a higher toxic burden which can look like, you know, fatigue, acne, hormone imbalance. We talk about this marker correlates so well that shows up on the DUTCH hormone test, if you’ve got crazy high estrogen. I just ended up having a male client who did.
He had really high estrogen and then high beta Glucuronidase. I’m like, well, here we go. Not that it is the one cause, there’s always multiple variables when we have some for whatever marker. But I really think this is a fascinating marker for explaining like, why someone’s toxic burden might be high, why they’re not able to bring their estrogen levels down.

It’s definitely something we want to address or talk about healing opportunity. If you’re recycling toxins, are you going to feel that great? Absolutely not. Are you going to gain the health that you want? Absolutely not. Again, with FDN, we want to reduce inflammation. We want to balance out the immune system, and we want to reduce or eliminate toxic burden.
I mean, everyone has some level of toxic burden in their body, whether it’s metals or mold or endotoxins from gut bugs or environmental toxins. We all have some level. But if you’ve got this high beta Glucuronidase marker, then your body’s just not getting it out the way it’s supposed to.
[00:36:15] Detective Ev: Sure. Well, what’s really cool about this, Becca, is I remember this at the time. Forgive me, what is it, calcium d-glucarate, is that something you could take temporarily? Am I saying that right?
Becca Kyle: Yeah.
Detective Ev: I used that along with Thorne, Liver Cleanse.
Supplements are Temporary Relief While Working on Lifestyle
What was nuts is I could so easily correlate only two days of use of this to lessening of skin symptoms. Now you don’t want to just treat.
What I mean by that is once I got to using it, like if I stopped for a day. I said that kind of wrong. Once I started using it, and I probably got a couple weeks in, if I stopped using it for a day or two, sure enough, right on the chin, another little breakout. Then if I started again, it would seem to support that. That’s really what I meant by the two days thing.
We’re not treating symptoms here because the supplements are great, but it’s more or less just a bandaid for the real problem. Thankfully, this did get addressed eventually, but it’s just kind of amazing how you can see this test.
No dermatologist has ever told me to look out for something like this or talk about my detox pathways or anything like it. Yet one of the cheapest supplements I ever bought was actually very supportive in helping me get some relief from that last little bit of acne before I really identified the bigger stuff that was leading to it.
That’s one of the beautiful things about being FDNs. We’re not going in and saying, oh, hey, just take the supplement for this high marker. No. We’re saying, hey, just so you know, if you can utilize this supplement for this high marker right now, it might give you some relief. We’re also going to work on what’s actually going on here so that you don’t need that supplement one day. That is a beautiful thing about being an FDN.
Gut Test Results: Secretory IgA
The next side here, one of the last things is the Immune Response, and we see Secretory IgA and Anti-gliadin IgA. My Secretory IgA is rather low. It is 192 on a reference range of 510 to 2010. What would your interpretation be of this, Becca, if I came to you back in 2018 and said, hey, here’s my test results?
[00:37:57] Becca Kyle: It’s so low. I want to see this at about a thousand. If I could just pick a perfect level, I would say about a thousand. You don’t want it too too low. You don’t want it too high, necessarily. Although if it’s high, that means your body’s doing something. It’s having probably an appropriate immune response for something.

We have the physical barrier of our gut lining. But the Secretory IgA is also, it’s a chemical barrier. It’s really the first line of defense in your gut against the things that we don’t want there that could potentially create a lot of issues.
This is showing that you potentially, maybe at one time, had high levels of Secretory IgA. I see that sometimes; it gets really high. You have this big immune response and then your body can’t keep up that immune response over time, so it starts tanking.
Some of the biggest reasons this number might be low is stress. High cortisol can decrease that Secretory IgA, but I often see it low with gut pathogens, with some of these opportunistic infections as well as things like food sensitives, like gluten, dairy, corn, some things that could be creating that immune response and that inflammatory response in the gut.
Gut Test Results: Anti-gliadin IgA
I would say that you definitely need some help here bringing up your Secretory IgA levels. Again, like Evan just said, there’s absolutely nothing wrong with creating a plan that’s got some allopathic care, that’s got some, hey, let’s get you feeling better quickly while we work on the root cause.
So, if all you’re doing is that allopathic care, let’s just get you feeling better without actually working on it, like, well, why is it low? What’s going on to cause it to be low? Then you’re never actually going to get the improvement that you want. So, I would say here, you know upping the levels of your Secretory IgA while we work on that root cause.
Now your Anti-gliadin is only 98. I would say though, if it’s above 50, then you’re having some sort of reactivity. Then with your Secretory IgA so low, I would really look at that Anti-gliadin as a false negative. You literally don’t have the immune response capacity to have the appropriate immune response to that Anti-gliadin marker.
By the way, it’s a gluten marker. So, I would call that gluten marker a false negative there because it’s above 50 and because your Secretory IgA is simply so low. I’ll often see gluten in a causative role for that low Secretory IgA.
[00:40:14] Detective Ev: This is a fairly simple example, but it’s one of the just million cool things we learn as FDNs where we look at the labs deeper and with more complexity than Western medicine does. Western medicine is actually not trained for the most part to analyze lab results, guys.
Gut Test Results: Calprotectin
Even if you could find a doctor that would run the GI MAP with you, which might be more likely than a lot of these other labs, but let’s say they did. It’s not that they can’t think of this, it’s not that complicated. But they are not trained to think about the idea that, oh, okay, the Anti-gliadin is a similar marker here in terms of like what is needed to create it.
So, if it’s within range, but the Secretory IgA is super low, oh, that would probably be a lot higher. Can we tell you how much higher? No, we can’t, but we can make a reasonable assumption that that is the case.
I have other tests to absolutely verify what you just said that I am in fact gluten-sensitive and so is my mom. This absolutely is again, really simple. Just one of the cool ways that we get trained as FDNs is different than any other practitioner out there to start looking at these little things that someone else could have the exact same test results in front of them and we’re going to find things and correlate things that other people just were simply not trained to do.
Last marker on here is Inflammation. We have Calprotectin. What is that marker? I’ve seen that very high in some people.
[00:41:31] Becca Kyle: It’s a marker for inflammation in the gut at the most basic level. It’s actually very studied and a very research marker. In my experience though, just because this marker might not be high, doesn’t mean you don’t have inflammation in your body. It’s more of like a gut specific marker here.
Gut Test Results: Occult Blood
Now if this marker was high and say your occult blood was high (Occult blood is a marker for blood in the stool.), I would refer someone out for a GI specialist. Let’s look, maybe get a colonoscopy. Let’s look for polyps. Let’s look for other things.
I often see the calprotectin and the occult blood high. I find that’s more common for me than just the calprotectin to be high. Do you find the same thing, Evan?
[00:42:11] Detective Ev: Yeah. I was distracted because one other thing I wanted to mention, we didn’t go over this on the occult blood, and we should have. Like if women have this, not high, but if it’s like a one, two, or three, we should have also said it’s not something to freak out about because a lot of the times the woman was on her period.
It might be someone that suffers from like hemorrhoids or, and not to be gross here, but we’re in the healthcare space, guys, you gotta be able to have mature conversations about this stuff. Some people, especially if their guts are messed up, they take really large poops. I would straight up ask them, hey, when you wipe, sometimes is there a little blood streak on it? Because that could be the occult blood there.
So, yes to your question. But then also I’m like thinking, dang, we should really mention that, just so people don’t freak out about occult blood if they saw it.
[00:42:50] Becca Kyle: No, I mean, the marker is in range under 10. I’ve seen it in the hundreds. I have a couple that was really crazy high.
Where to Find Becca Kyle
So yeah, what I love about this test, this just overall test, is you can correlate to so many of the things, the health challenges you’ve been experiencing. I always tell my clients; we can do something about all of it. You’re not stuck feeling the way you feel, and so many people feel like they’re stuck, but you’re not. This has so many actionable steps that can be taken out of it. I love this test.
[00:43:17] Detective Ev: Cool. Well, I appreciate you going over this with me. We like nailed the timing. That was kind of unintentional. I couldn’t even see what it was.
Now with that all said, if you guys are interested in like actually learning how to analyze labs like this, this is just the tip of the iceberg for what we get to learn as FDNs.
If you’re wanting to learn more about FDN, you can go to fdntraining.com/tryfdn, and it’ll allow you to try the course for free.
But maybe you’re like, all right, cool. I thought this was awesome, but I’m not necessarily trying to be the person who goes out and does this stuff. I want to learn from someone who does this. Becca, where can they find you? Because I know you utilize this lab all the time as well as many others in your practice.

[00:43:54] Becca Kyle: Yeah, I do. So, if you just want to connect with me, my brand is Holistic Obsession. You can find me at holisticobsession.com. I have a private but free Facebook group. There’d be a link to that from my website. If you just want to chit chat, I offer free connection calls.
Conclusion
I just love connecting with people and really being able to have a conversation about what’s possible for your health. So, again, on the website, there’ll be a button to schedule that free connection call. We can just have a conversation cause most people don’t really know what’s possible, how good they’re meant to feel, and how good they have the potential to feel with the right data and the right action steps.
[00:44:28] Detective Ev: We will have all those links for you guys in the show notes and then in the YouTube description as well, of course. But Becca, thank you so much for coming on with me and helping me continue this series where we get to really show off what we get to do as FDNs.
[00:44:39] Becca Kyle: It’s so much fun. Thank you for having me on. I appreciate it.
You can always visit us at functionaldiagnosticnutrition.com.
To hire a coach, go to fdnthrive.com.
For a FREE Health Review, go to fdnthrive.com/match/.